How do I know if my acne is bacterial or hormonal?
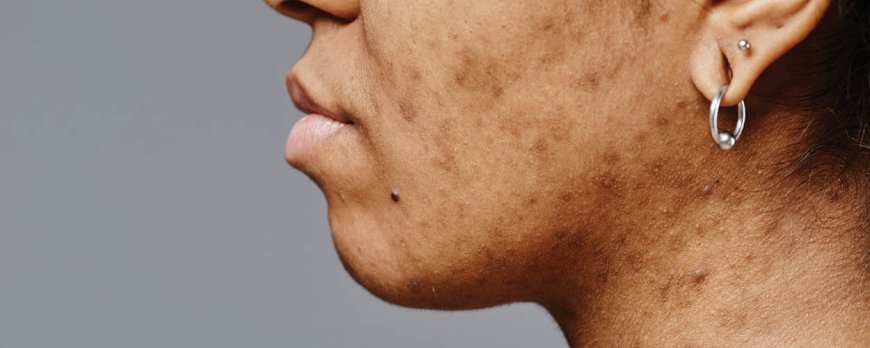
Unlock the mystery of your acne. Discover 'How do I know if my acne is bacterial or hormonal?' to determine the best solution for your skincare.
How do I know if my acne is bacterial or hormonal?
Determining the cause of your acne is crucial in finding the most effective treatment. Understanding whether your acne is bacterial or hormonal can help you tailor your skincare routine and choose the right products to address the underlying issue.
Key Takeaways:
- Hormonal acne is triggered by hormonal fluctuations and typically manifests as deep red and tender cysts.
- Bacterial acne is an inflammatory reaction caused by bacterial overgrowth, inflammation, and increased sebum production.
- Consulting a dermatologist is essential for a proper diagnosis and individualized treatment plan.
- Treatment options for hormonal acne may include topical anti-inflammatory medications, birth control pills, spironolactone, and a consistent skincare routine.
- Treatment options for bacterial acne may involve benzoyl peroxide, retinoids, antibiotics, and antifungal treatments for fungal acne.
Differentiating bacterial and hormonal acne
Bacterial and hormonal acne have distinct characteristics that can help in identifying the type of acne you may be experiencing. Hormonal acne is typically triggered by hormonal fluctuations and is often characterized by deep red and tender cysts. It commonly appears in the lower parts of the face, such as the jawline, chin, neck, or cheeks. This type of acne is caused by the skin's sensitivity to male dominant hormones called androgens, which stimulate oil glands to overproduce oil, leading to the overgrowth of acne-causing bacteria.
On the other hand, bacterial acne is an inflammatory reaction caused by a combination of bacterial overgrowth, inflammation, and increased sebum production. It manifests as red or pus-filled pimples that can be painful to touch. Bacterial acne can occur on various parts of the face, including the forehead, nose, and cheeks. It is often accompanied by an oily complexion and can lead to the formation of acne scars if not treated properly.
When determining the type of acne you have, it's important to consider the location, appearance, and any accompanying symptoms. Hormonal acne is often deeper and more cystic, while bacterial acne tends to be more surface-level and inflammatory. Consulting a dermatologist can provide a more accurate diagnosis and help you explore suitable treatment options based on your individual condition.
In summary, understanding the differences between bacterial and hormonal acne can guide you in identifying the specific type of acne you are dealing with. This knowledge is crucial for developing an effective skincare routine and seeking appropriate treatment options to manage and improve your skin condition.

Causes of Hormonal Acne
Hormonal acne is primarily caused by hormonal imbalances in the body, specifically related to androgens and oil production. When androgens, which are male dominant hormones, are present in excess amounts, they stimulate the oil glands to produce more oil than necessary. This overproduction of oil, known as sebum, can clog the pores and create a favorable environment for the growth of acne-causing bacteria.
In addition to excess oil production, hormonal acne can also be triggered by fluctuations in hormone levels. This commonly occurs during puberty, menstruation, pregnancy, or menopause. The fluctuations in estrogen and progesterone levels can disrupt the balance in the skin, leading to the development of acne.
Furthermore, certain lifestyle factors can contribute to hormonal imbalances and subsequently, hormonal acne. Factors such as chronic stress, inadequate sleep, an unhealthy diet, and the use of certain medications or cosmetic products can influence hormone levels and increase the likelihood of developing hormonal acne.
Factors contributing to hormonal acne:
- Hormonal imbalances related to androgens
- Excess oil production
- Fluctuations in hormone levels during puberty, menstruation, pregnancy, or menopause
- Chronic stress
- Inadequate sleep
- Unhealthy diet
- Use of certain medications or cosmetic products
Understanding the underlying causes of hormonal acne is crucial in determining the appropriate treatment options. By addressing the hormonal imbalances and implementing lifestyle changes, individuals can manage and improve their acne condition effectively.
Causes of Bacterial Acne
Bacterial acne occurs as a result of a combination of factors, including bacterial overgrowth, inflammation, and excess sebum production. When the hair follicles become clogged with dead skin cells and sebum, the ideal environment is created for the growth of acne-causing bacteria, such as Propionibacterium acnes.
This bacterial overgrowth triggers an immune response, leading to inflammation and the formation of red, swollen acne lesions. Additionally, the increased production of sebum, the skin's natural oil, further contributes to the development of bacterial acne.
H3: Factors contributing to bacterial acne:
- Poor hygiene and infrequent cleansing, which can allow bacteria to thrive
- Excessive sebum production due to hormonal imbalances or genetic predisposition
- Inflammation caused by the body's immune response to bacterial activity
- Environmental factors, such as pollution or exposure to certain chemicals
To effectively treat bacterial acne, it is important to eliminate or reduce the factors that contribute to its development. This includes maintaining good hygiene practices, using non-comedogenic skincare products, and adopting a consistent cleansing routine. In more severe cases, dermatologists may prescribe topical treatments containing ingredients like benzoyl peroxide or retinoids to combat bacteria, reduce inflammation, and promote the exfoliation of dead skin cells.
By understanding the causes of bacterial acne and implementing appropriate treatment measures, individuals can effectively manage their condition and improve the health and appearance of their skin.
Consult a dermatologist for a proper diagnosis
To determine whether your acne is bacterial or hormonal, it is essential to consult a dermatologist who can provide a professional diagnosis. They have the expertise to assess your acne and consider various factors like appearance, location, and medical history to determine the underlying cause. In some cases, they may recommend additional tests, such as bloodwork or pore analysis, to further evaluate hormonal levels and bacterial composition.
Why is a dermatologist consultation necessary?
- A dermatologist can accurately differentiate between bacterial and hormonal acne, as they have an in-depth understanding of the characteristics and triggers of each type.
- They can tailor treatment options to your specific acne type, ensuring effective management and minimizing the risk of further complications.
- Professional guidance can prevent self-diagnosis mistakes and incorrect treatment choices, which may worsen the condition or delay improvement.
It is crucial to seek a dermatologist's expertise for an accurate diagnosis, especially when facing persistent or severe acne. They can provide personalized treatment plans, taking into account your unique skin needs, medical history, and lifestyle factors. Remember that each individual's acne journey is different, and a dermatologist can guide you towards the most suitable treatment options to help improve your skin condition.
By collaborating with a dermatologist, you can gain a deeper understanding of your acne, explore effective treatment options, and work towards achieving clearer, healthier skin.
Treatment options for hormonal acne
Managing hormonal acne involves a variety of treatment approaches, including topical medications, hormonal regulation, and maintaining a proper skincare routine. Here are some options to consider:

1. Topical anti-inflammatory medications
Topical medications containing ingredients like benzoyl peroxide, salicylic acid, or retinoids can help reduce inflammation and control acne breakouts. These products work by unclogging pores, reducing oil production, and promoting skin cell turnover.
2. Hormonal regulation
For individuals with hormonal acne, regulating hormone levels can be an effective treatment strategy. This may involve using oral contraceptives (birth control pills) that contain estrogen and progestin to balance hormone fluctuations. Another medication option is spironolactone, which blocks androgen receptors to reduce oil production.
3. Consistent skincare routine
Establishing a consistent skincare routine can help manage hormonal acne. This includes cleansing the skin twice a day with a gentle cleanser, using non-comedogenic moisturizers and sunscreen, and avoiding harsh or abrasive skincare products that can irritate the skin and worsen acne.
It's important to note that finding the right treatment option for hormonal acne may require some trial and error, as what works for one person may not work for another. It's best to consult with a dermatologist who can evaluate your specific condition and recommend the most suitable treatment approach.
Treatment options for bacterial acne
Effective treatment for bacterial acne often involves a combination of topical and oral medications tailored to address the underlying causes of inflammation and bacterial overgrowth. Here are some commonly used treatment options:
- Benzoyl peroxide: This topical medication works by killing bacteria on the skin, reducing inflammation, and unclogging pores. It is available over-the-counter in various strengths and forms, such as gels, creams, and cleansers.
- Retinoids: These vitamin A derivatives are available as topical creams or gels and work by unclogging pores and preventing the formation of new acne lesions. They also have anti-inflammatory properties and can help fade acne scars over time.
- Antibiotics: Oral antibiotics, such as tetracycline or erythromycin, may be prescribed to target the bacteria causing the acne. These medications help reduce inflammation and control the growth of bacteria. It is important to follow the prescribed dosage and complete the full course of antibiotics.
- Antifungals: In cases where the acne is caused by a fungal infection, antifungal medications may be prescribed. These medications work by killing the fungus and reducing inflammation. They may be used in combination with other topical or oral treatments.
It's essential to consult a dermatologist to determine the most suitable treatment options for your bacterial acne. They can evaluate your specific condition, consider any underlying factors, and provide personalized recommendations. In addition to medication, maintaining a consistent skincare routine, practicing good hygiene, and avoiding picking or squeezing acne lesions can help improve the effectiveness of the treatment and prevent further breakouts.
Lifestyle factors and acne
Lifestyle factors play a significant role in managing acne, and paying attention to sleep, stress, hydration, and diet can contribute to improved skin health.
1. Sleep: Getting enough sleep is crucial for overall well-being, including skin health. Lack of sleep can lead to increased stress levels and hormonal imbalances, which can worsen acne. Aim for 7-9 hours of quality sleep each night to promote healthy skin.
2. Stress management: Stress can trigger hormonal fluctuations, leading to the onset or worsening of acne. Finding effective stress management techniques like exercise, meditation, or hobbies can help reduce stress levels and improve acne symptoms.
3. Hydration: Staying hydrated is essential for maintaining healthy skin. Drinking an adequate amount of water helps flush out toxins and keeps the skin hydrated, reducing the risk of clogged pores and acne breakouts.
4. Diet: While diet alone may not be the main cause of acne, certain foods can exacerbate symptoms. Limiting dairy and high-sugar foods can help reduce inflammation and regulate oil production, leading to clearer skin. Incorporating foods rich in antioxidants, vitamins, and minerals, such as fruits, vegetables, and whole grains, can support skin health.
By incorporating these lifestyle factors into your daily routine, you can support the management of acne and promote healthier skin. However, it's important to remember that individual responses may vary, and consulting with a dermatologist is always recommended for a comprehensive acne management plan.
Conclusion
Understanding the difference between bacterial and hormonal acne is key to effectively managing and improving your skin condition. By considering certain factors, you can determine whether your acne is caused by hormonal fluctuations or bacterial overgrowth.
Hormonal acne is characterized by deep red and tender cysts, often appearing in the lower parts of the face such as the jawline, chin, neck, or cheeks. It is triggered by the skin's sensitivity to androgens, male dominant hormones that stimulate oil glands to overproduce oil. This overproduction of oil leads to the overgrowth of acne-causing bacteria.
On the other hand, bacterial acne is an inflammatory reaction caused by a combination of bacterial overgrowth, inflammation, and increased sebum production. It manifests as red, inflamed pimples and may spread across different areas of the face.
To receive a proper diagnosis and explore suitable treatment options, it is recommended to consult a dermatologist. They can assess your acne, conduct a thorough examination, and consider your medical history. They may also suggest a blood test to evaluate hormone levels or analyze the composition of bacteria in your pores.
Treatment options for hormonal acne may include topical anti-inflammatory medications, birth control pills, spironolactone, a consistent skincare routine, and the use of non-comedogenic products. For bacterial acne, treatment options may involve benzoyl peroxide, retinoids, antibiotics, and antifungals if the acne is fungal in nature.
In addition to seeking professional help and considering appropriate treatment options, it is important to pay attention to lifestyle factors that can impact acne. This includes prioritizing sufficient sleep, managing stress levels, staying hydrated, and limiting dairy and sugar intake.
By understanding the underlying cause of your acne and implementing suitable measures, you can effectively manage and improve your skin condition, ultimately achieving a clearer and healthier complexion.

FAQ
How do I know if my acne is bacterial or hormonal?
To determine whether your acne is bacterial or hormonal, you should consult a dermatologist who can assess your acne, conduct a thorough examination, and consider your medical history. They may also suggest a blood test to evaluate hormone levels or examine the composition of bacteria in your pores.
What are the characteristics of hormonal acne?
Hormonal acne is often characterized by deep red and tender cysts. It commonly appears in the lower parts of the face, such as the jawline, chin, neck, or cheeks.
What are the characteristics of bacterial acne?
Bacterial acne is an inflammatory reaction caused by a combination of bacterial overgrowth, inflammation, and increased sebum production.
What causes hormonal acne?
Hormonal acne is caused by the skin's sensitivity to male dominant hormones called androgens, which stimulate oil glands to overproduce oil, leading to the overgrowth of acne-causing bacteria.
What causes bacterial acne?
Bacterial acne is caused by a combination of bacterial overgrowth, inflammation, and increased sebum production.
How can a dermatologist help with acne diagnosis?
A dermatologist can accurately diagnose the type of acne by assessing your acne, conducting a thorough examination, considering your medical history, and potentially suggesting additional tests.
What are the treatment options for hormonal acne?
Treatment options for hormonal acne can include topical anti-inflammatory medications, birth control pills, spironolactone, consistent skincare routine, and non-comedogenic products.
What are the treatment options for bacterial acne?
Treatment options for bacterial acne may include benzoyl peroxide, retinoids, antibiotics, and treating fungal acne with antifungals.
Can lifestyle factors impact acne?
Yes, lifestyle factors such as getting enough sleep, managing stress, staying hydrated, and limiting dairy and sugar intake can impact acne.



































































































































